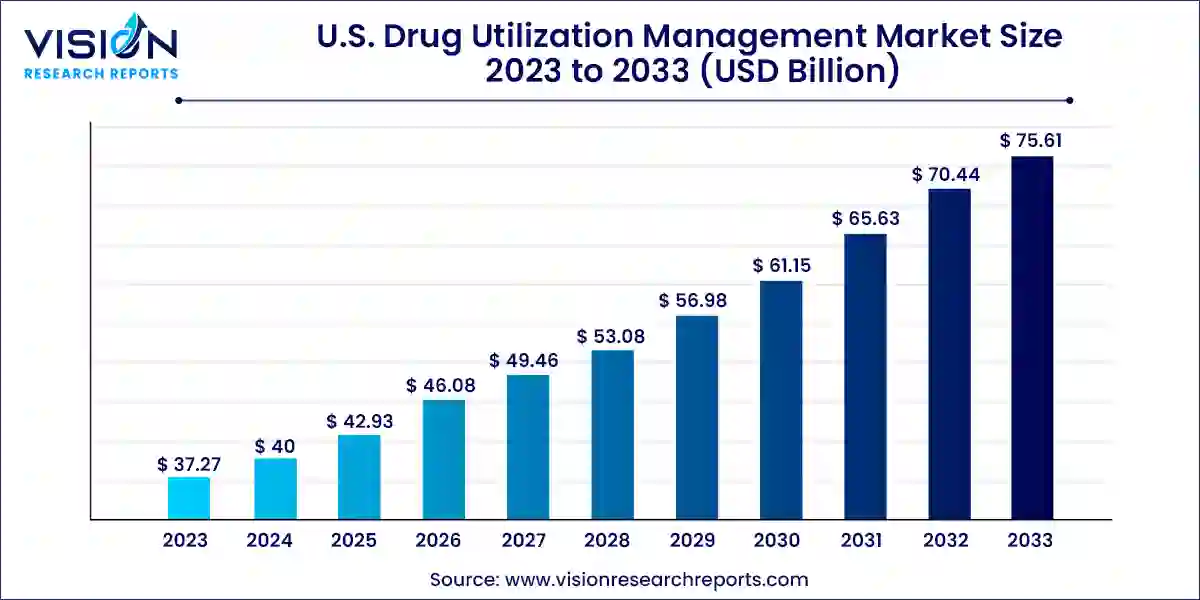
The U.S. drug utilization management market size was valued at USD 37.27 billion in 2023 and it is predicted to surpass around USD 75.61 billion by 2033 with a CAGR of 7.33% from 2024 to 2033.
Key Pointers
- By Program Type, the in-house segment held the largest revenue share of 66% in 2023.
- By Program Type, the outsourced segment is anticipated to experience rapid growth throughout the forecast period.
- By End-use, the PBMs segment generated the maximum market share of 38% and is projected to exhibit the highest growth rate from 2024 to 2033.
- By End-use, the health plan provider/payors segment is expected to witness significant growth in the forecast period.
Introduction to Drug Utilization Management (DUM)
Drug Utilization Management (DUM) refers to a set of strategies used by healthcare providers, insurers, and pharmaceutical companies to ensure that medications are used appropriately and effectively. This includes controlling costs, promoting patient safety, and optimizing therapeutic outcomes through various mechanisms.
Get a Sample@ https://www.visionresearchreports.com/report/sample/41416
U.S. Drug Utilization Management Market Dynamics
Drivers
- Rising Healthcare Costs: With healthcare expenditures continually increasing, there is a growing need for cost-containment strategies such as DUM to manage pharmaceutical expenditures effectively.
- Advancements in Technology: Technological innovations like data analytics, AI, and machine learning are enhancing the effectiveness and efficiency of DUM programs, leading to better patient outcomes and cost savings.
- Regulatory Mandates: Stringent regulatory requirements from bodies like CMS (Centers for Medicare & Medicaid Services) and private insurers drive adoption of DUM practices to ensure compliance and quality of care.
Challenges
- Complexity of Healthcare Ecosystem: Integration of DUM programs into existing healthcare systems can be challenging due to the complexity of workflows, interoperability issues, and varying stakeholder interests.
- Patient Adherence and Engagement: Ensuring patient adherence to DUM protocols and fostering engagement requires overcoming barriers such as lack of awareness, resistance to change, and communication gaps between providers and patients.
- Data Privacy and Security Concerns: Handling sensitive patient data within DUM systems necessitates robust security measures to protect against breaches, complying with stringent privacy regulations like HIPAA.
Opportunities
- Expansion of Value-Based Care Models: The shift towards value-based care provides opportunities for DUM to demonstrate its role in improving health outcomes, reducing costs, and enhancing patient satisfaction.
- Personalized Medicine: The trend towards personalized medicine creates opportunities for DUM to tailor interventions based on patient-specific factors such as genetics, lifestyle, and treatment history, thereby optimizing therapy outcomes.
- Telehealth and Digital Health Integration: The rise of telehealth and digital health solutions presents opportunities to integrate DUM seamlessly into virtual care environments, enhancing accessibility and continuity of care while leveraging real-time data analytics.
Segmentation Insights
- By Type of Utilization Management:
- Prior Authorization: This involves obtaining approval from insurers or pharmacy benefit managers (PBMs) before certain medications are dispensed to patients. It aims to ensure appropriate and cost-effective medication use.
- Step Therapy: This requires patients to try less expensive or preferred drugs before moving to more costly alternatives, promoting cost containment.
- Quantity Limits: Setting limits on the amount of medication a patient can receive over a specified period, which helps control costs and prevent misuse.
- By End-User:
- Healthcare Providers: Including hospitals, clinics, and physician practices that implement DUM programs to manage medication use among their patient populations.
- Payers (Insurers and PBMs): These entities administer DUM strategies to control drug costs, improve patient safety, and ensure appropriate utilization across their covered populations.
- Patients: Increasingly involved in DUM decisions, especially with the rise of shared decision-making and patient-centered care models.
- By Therapeutic Area:
- Chronic Diseases: Such as diabetes, hypertension, and cardiovascular diseases, where DUM focuses on ensuring adherence to treatment guidelines and optimizing medication therapies.
- Specialty Drugs: High-cost medications used to treat complex conditions like cancer, autoimmune disorders, and rare diseases, requiring stringent management to ensure appropriate use and cost-effectiveness.
- Mental Health and Behavioral Disorders: Where DUM strategies address medication adherence, appropriate dosing, and the integration of behavioral health with primary care.
- By Technology Platform:
- Software Solutions: DUM platforms often integrate with electronic health records (EHRs) and pharmacy management systems to streamline authorization processes, monitor adherence, and analyze utilization patterns.
- Analytics and Reporting Tools: Utilized to track medication utilization trends, monitor patient outcomes, and identify opportunities for improvement in care delivery and cost management.
- Telehealth and Digital Health Solutions: Facilitating remote patient monitoring, virtual consultations, and medication adherence support, enhancing the effectiveness of DUM initiatives.
Read More@ https://www.heathcareinsights.com/asia-pacific-viral-vector-and-plasmid-dna-manufacturing-market/
U.S. Drug Utilization Management Market Key Companies
Third Party Providers:
- Prime Therapeutics LLC
- MedicusRx
- EmblemHealth
- Optum, Inc.
- Point32Health, Inc.
- AssureCare LLC
- MindRx Group
- Agadia Systems, Inc
- Elevance Health (CarelonRx)
- ExlService Holdings, Inc.
- MRIoA
- S&C Technologies, Inc.
In-House Providers:
- Ultimate Health Plans
- Security Health Plan of Wisconsin, Inc.
- Blue Cross and Blue Shield Association
- Providence
- Simply Healthcare Plans, Inc
- Health Plan of San Mateo (HPSM)
- PerformRx
- Aetna, Inc. (CVS Health Corp.)
U.S. Drug Utilization Management Market Segmentation:
By Program Type
- In-house
- Outsourced
By End-use
- PBMs
- Health Plan Provider/Payors
- Pharmacies
Buy this Premium Research Report@ https://www.visionresearchreports.com/report/checkout/41416
You can place an order or ask any questions, please feel free to contact sales@visionresearchreports.com| +1 650-460-3308
Web: https://www.visionresearchreports.com/
Blog: https://www.novaoneadvisor.com/
